As of late, the field of cancer treatment has been focusing on multidrug therapy in clinical trial research.
Scientists are deepening their understanding of cancer's intricate biology by resorting to novel approaches that combine therapeutic agents currently developed to target multiple pathways concurrently.
These advancements promise to yield more efficacious treatment outcomes, especially for cancers that exhibit resistance to conventional monotherapies.
Current clinical trial research emphasizes optimizing these drug combinations and customizing treatments to align with the distinctive genetic profiles of individual patients, thereby heralding a new era in cancer care.
Advances in Multidrug Approaches for Treating Cancer
Multidrug therapy, involving the combination of several therapeutic agents, has transformed cancer treatment by targeting multiple pathways in tumor growth and survival.
Traditional treatments, such as monotherapies, often result in resistance due to cancer's adaptability, but multidrug approaches can suppress multiple resistance mechanisms at once.
Recent advancements have focused on developing multi-targeted drugs (MTDLs) that simultaneously act on several biological targets.
These therapies, such as those using receptor tyrosine kinase (RTK) inhibitors and JAK/STAT pathway modulators, have demonstrated efficacy in treating a wide range of cancers, including breast, lung, and liver.
These targeted therapies have shown success by disrupting critical signaling pathways that cancer cells rely on to proliferate and spread.
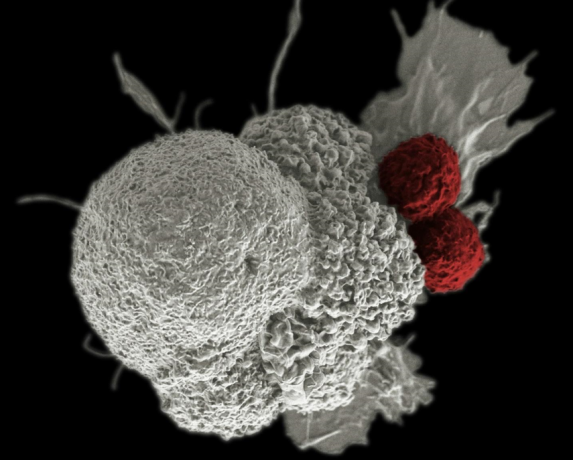
Furthermore, the rise of immunotherapy combined with chemotherapy and targeted treatments has opened new possibilities: For example, CAR-T cell therapy, which reprograms a patient's immune cells to attack cancer, is being explored in combination with other drugs to increase treatment efficacy in solid tumors.
Overcoming Resistance and Side Effects in Cancer Multidrug Therapy
One of the most significant challenges in cancer therapy is drug resistance, where cancer cells adapt and evolve to render treatment ineffective.
Multidrug therapy helps to counter this issue by using drugs with different mechanisms of action, making it harder for cancer cells to develop resistance simultaneously to all agents used.
However, the complexity of combining therapies can also introduce new challenges, such as increased toxicity and side effects.
Innovative drug delivery systems, like nanoparticle-based delivery, are being researched to ensure drugs reach the tumor site more precisely, reducing off-target effects and minimizing toxicity.
By delivering drugs more efficiently, these systems reduce the dose required and limit side effects while maintaining or improving therapeutic efficacy.
Researchers have also focused on optimizing drug combinations through computational modeling and AI-driven simulations.
These tools help to predict how different drugs interact, reducing the risk of adverse effects and identifying the most effective combinations.
The Role of Personalized Medicine in the Evolution of Multidrug Cancer Therapies
Personalized medicine is transforming cancer treatment by tailoring therapies to a patient's tumor's unique genetic makeup.
Advances in genomic sequencing and molecular profiling allow oncologists to select drug combinations that target specific mutations and pathways within the cancer, ensuring a more effective and individualized approach.
In the context of multidrug therapy, personalized medicine is crucial in determining the optimal combination of drugs for each patient: For instance, tumors with specific genetic mutations, such as those affecting the BRCA genes in breast and ovarian cancers, can be targeted with drugs like PARP inhibitors combined with chemotherapy.
Moreover, as our understanding of cancer biology deepens, the ability to design more refined treatment regimens based on a patient's biomarker profile will only increase.
Biomarkers help predict how a patient will respond to a particular drug or combination of drugs, allowing for a more precise approach to cancer treatment.
This therapy tailoring improves outcomes and minimizes unnecessary side effects, as patients are less likely to be treated with ineffective drugs.
Future Directions for Multidrug Cancer Therapies
The future of cancer treatment lies in the continued integration of multidrug therapies with precision medicine.
Clinical trials will increasingly focus on identifying the best drug combinations for specific cancer types and genetic profiles.
Using real-time patient data, such as from wearable devices and AI-powered health tracking, will enable more adaptive treatment plans that respond dynamically to how a patient's cancer evolves.
Another promising avenue is using biomarkers to monitor resistance in real time – this would allow oncologists to modify a treatment plan at the earliest signs of resistance, shifting to a new combination of drugs before the cancer can progress further.
As research continues, the challenge will be ensuring these advanced therapies remain accessible and affordable to all patients; healthcare systems must adapt to support the delivery of complex multidrug regimens, especially as treatments become increasingly personalized and technology-driven.
In Conclusion
Multidrug therapy is revolutionizing the way we approach cancer treatment, offering hope for more effective, personalized, and less toxic therapies.
Clinical trial research will continue to explore new drug combinations, overcome resistance, and refine the use of biomarkers, which means we are likely to see even more breakthroughs in years to come.
By leveraging the power of personalized medicine and novel delivery systems, the future of cancer treatment looks brighter, with improved survival rates and quality of life for patients.