Fungal infections can be an uncomfortable and persistent problem. While many minor fungal infections can be treated with over-the-counter remedies, some signs indicate that professional medical attention is needed. Identifying these signs early can prevent the condition from worsening and spreading.
Here are 11 signs your fungal infection needs professional treatment.
Persistent Itching and Discomfort
If you experience unrelenting itchiness that doesn't improve with over-the-counter treatments, it's time to seek medical help. Common areas affected include the feet, groin, and under the breasts.
Persistent itching can indicate a more severe infection that requires stronger medication. Persistent itching and discomfort are not only irritating but also a clear signal that the fungal infection is not responding to initial treatments.
Over-the-counter creams and ointments are designed to handle minor cases, but when these symptoms persist, it could mean that the infection is more entrenched and resistant. This persistence often leads to significant discomfort that can disrupt daily activities and affect your quality of life.
Seeking professional medical advice is crucial at this stage to prevent the infection from spreading further and to find a more effective treatment solution.
Spread of the Infection
An infection that spreads to other parts of the body despite treatment is a clear sign of a more severe problem. Prompt treatment is essential to prevent further rapid progression of the infection.
The spread of the infection is concerning, particularly when it reaches previously unaffected regions. This indicates that fungal spores are not being adequately controlled, potentially escalating into a more extensive problem. New symptoms and complications may arise, complicating treatment.
Professional intervention is essential to halt the spread and to develop a comprehensive treatment plan. Before addressing these challenges, consider the effectiveness of purehealth fungus eliminator. This product has shown promising results in overcoming the spread of fungal infections by targeting and eliminating the spores, providing a robust solution to manage and resolve such health issues.
Severe Redness and Swelling
Intense redness, swelling, or inflammation that worsens over time could indicate a more severe fungal infection or even a secondary bacterial infection. These symptoms require urgent medical attention.
Severe redness and swelling are clear indicators that the body's immune response is in overdrive, trying to combat the infection. This level of inflammation can cause significant discomfort and might suggest that the infection has penetrated deeper into the skin layers or even into other tissues.
Ignoring these symptoms can lead to more severe health issues, including secondary bacterial infections that can complicate treatment. Medical professionals can provide the necessary interventions to reduce inflammation and address any secondary infections that might be present.
Painful Cracks or Sores
The development of painful cracks, sores, or ulcers in the infected area is a serious sign. These symptoms can lead to secondary infections and delayed healing, necessitating professional intervention. Painful cracks and sores can significantly impact your daily activities, especially if they affect your feet or hands.
These open wounds are also vulnerable to additional infections, as bacteria can easily enter and cause further complications. The pain associated with these symptoms can be severe, indicating that the infection is causing significant tissue damage.
Pus or Discharge
The presence of pus or any abnormal discharge from the infected area indicates a severe fungal infection that requires medical attention. Ignoring this sign can lead to further complications.
Pus or discharge is a clear sign that the body is fighting off a significant infection. This symptom usually indicates that there is an accumulation of dead cells, bacteria, and immune cells, suggesting that the infection is severe.
The presence of pus often accompanies a foul smell and can lead to increased pain and discomfort. Seeking medical attention is critical to properly clean the infected area, remove any dead tissue, and administer the appropriate medications to eliminate the infection.
Fever and Malaise
Fever, fatigue, or a general feeling of being unwell accompanying the infection are signs that the infection might be spreading or affecting your body systemically. This requires prompt medical evaluation.
Fever and malaise indicate that the infection is not localized but is affecting the body's overall health. A fever is the body's natural response to fighting an infection, but when it accompanies a fungal infection, it suggests that the immune system is struggling to contain the spread.
Feeling generally unwell or fatigued can make it difficult to carry out everyday activities and can indicate that the body is using a lot of energy to fight off the infection. Professional medical evaluation is necessary to determine the extent of the infection and to provide the appropriate systemic treatments.
Failure to Improve with OTC Treatments
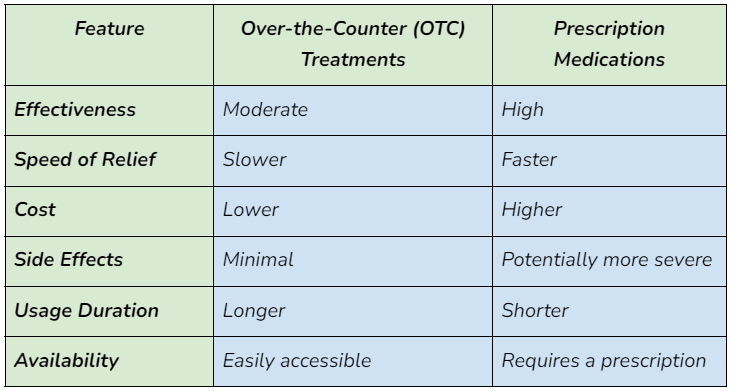
If there is a lack of improvement after using over-the-counter antifungal creams or medications, it may be time to consider stronger prescription medications. Persistent symptoms indicate that the infection might be resistant to OTC treatments.
Over-the-counter treatments are typically effective for mild fungal infections, but when there is no improvement, it suggests that the infection is more resilient. This failure to respond to standard treatments can lead to prolonged discomfort and an increased risk of spreading the infection.
Prescription medications are often more potent and can target the infection more effectively. Consulting with a healthcare provider can provide access to these stronger treatments and a more tailored approach to managing the infection.
Recurring Infections
Frequent recurrence of fungal infections after initial treatment can indicate underlying conditions or immune system issues that need to be addressed. Professional treatment can help manage these recurrent infections more effectively.
Recurring infections are frustrating and can indicate that the underlying issue has not been fully resolved. This recurrence might be due to incomplete treatment, re-exposure to the fungus, or an underlying health condition that predisposes you to infections.
Identifying and addressing these underlying causes is crucial to breaking the cycle of recurrence. A healthcare provider can help diagnose any underlying conditions and provide a comprehensive treatment plan to prevent future infections.
Nail Involvement
Thickening, discoloration, or crumbling of nails are indicators of a severe fungal nail infection. Treating nail fungus can be challenging, and professional help is often required for effective treatment.
Fungal nail infections, also known as onychomycosis, can be particularly stubborn and difficult to treat with over-the-counter remedies. These infections cause the nails to become thick, discolored, and brittle, often leading to pain and difficulty in performing daily tasks.
The nails may crumble and become unsightly, affecting self-esteem and comfort. Professional treatment options, such as prescription medications or specialized procedures, are often necessary to effectively treat fungal nail infections and restore healthy nails.
Affecting Scalp or Hair Loss
Fungal infections of the scalp leading to hair loss or scalp sores need special consideration. These infections are difficult to treat and require professional medical care to prevent permanent damage.
Scalp fungal infections, known as tinea capitis, can cause hair loss and painful sores on the scalp. These infections can spread quickly and are particularly common in children.
The hair loss associated with these infections can be distressing and can lead to permanent scarring if not treated promptly. Professional treatment is essential to eradicate the infection and to prevent further hair loss and scarring.
Compromised Immune System
Individuals with weakened immune systems, such as those with diabetes or HIV, experiencing more severe or frequent fungal infections need professional treatment. Their immune system's inability to fight infections requires more robust medical interventions.
A compromised immune system makes it difficult for the body to fend off infections, making fungal infections more severe and frequent. Conditions like diabetes, HIV, or treatments such as chemotherapy can weaken the immune system, increasing the risk of severe fungal infections.
For these individuals, professional treatment is critical to manage infections effectively and to prevent complications. A healthcare provider can offer specialized treatments and monitor the infection closely to ensure proper management.
Over-the-Counter vs. Prescription Antifungal Treatments
Wrap Up
Fungal infections, while often minor, can escalate and become serious health concerns if not properly treated. By recognizing the signs that require professional treatment, you can ensure timely and effective management of these infections.
Don't ignore persistent symptoms; seeking medical advice can prevent complications and promote quicker recovery.
FAQs
1. Can I treat a fungal infection at home?
Yes, minor infections can be treated with OTC remedies, but persistent or severe symptoms need professional care.
2. How long do fungal infections take to heal?
Healing times vary; mild infections may clear in weeks, while severe cases can take months and require medical treatment.
3. What are the risks of untreated fungal infections?
Untreated infections can spread, become more severe, and lead to secondary bacterial infections. Seek professional treatment for persistent symptoms.
By focusing on these critical signs, you can better understand when it's crucial to seek professional treatment for a fungal infection. Early intervention can prevent complications and ensure a smoother recovery.






